A Physiotherapists Guide to Treating Tennis Elbow
Are you struggling with pain on the outside of your elbow? If so, you might have tennis elbow!
Tennis elbow (clinically known as lateral epicondylitis), is a common overuse injury that affects the tendons and muscles in the outer part of the elbow. Despite its name, it can occur not only in tennis players, but also in individuals who perform repetitive arm movements, such as painters, plumbers, and even computer users.
Tennis elbow typically presents as pain and tenderness on the outer side of the elbow, which can radiate down the forearm. People experiencing tennis elbow often describe sensations of sharp pain on the outside of the elbow, numbness down the the top of the forearm, weakness through the arm when lifting things (like milk jugs or cups of coffee), and sometimes feel like their fingers are “stiff” or hard to move.
When people develop tennis elbow, they essentially have created small tears in the muscles and tendons that attach to the outside of the elbow. These mirco-tears will cause serious pain until they heal - which leads to the soreness that you feel with tennis elbow.
These small muscles on the outside of the forearm can cause major problems when they are injured. Simple things like typing at the computer is no longer possible. Pickleball or tennis becomes unmanageable. Even pouring a cup of coffee becomes a mountain of discomfort to overcome.
Having tennis elbow is not fun, but fortunately our team here at MOMENTUM Physical Therapy are experts and are here to help!
Before we go any further, let me introduce myself. My name is Stephen Uhrbach and I am a physical therapist at MOMENTUM Physical Therapy in Okotoks, Alberta.
Our team here at MOMENTUM Physical Therapy understands the frustrations that come with tennis elbow and we are dedicated to get you back to your best. We are known for providing personalized care to help you recover swiftly and effectively.
In this blog post, we'll dive into how MOMENTUM Physical Therapy can use tailored physical therapy techniques to assist you in overcoming tennis elbow and getting back to doing what you love pain-free.
Let's start off by walking our way through helping you heal your tennis elbow.
Step 1: Reduce Your Pain
Having pain is miserable. The first step in your recovery is to reduce your pain. How do we do this?
Heat and/or ice
Using heat or ice depends on how new the tennis elbow injury is.
If you recently injured your elbow (think less then 10-14 days ago), you will be looking to ice the elbow. In this case, the injuries to the outside of the elbow are fresh and we are looking to manage swelling. Use an ice pack with a damp cloth between the skin and the ice pack for 20 minutes a time 2-3 times per day.
If your elbow injury is a little older in nature (think >14 days ago), heat will likely be your best friend. In this case, the inflammation is usually reduced in the elbow and we need to increase blood flow to the injured tendons to promote healing.
2. Bracing
You can purchase an over the counter tennis elbow brace. These braces are designed to help take the load off the injured tendon to allow it to rest and heal.
NOTE - wearing a brace for longer then 2-4 weeks is not recommended as the arm will become dependent on the brace. The goal of the brace is to rest the injured tendon for 2-4 weeks to allow it to heal.
3. Resting
Taking a break from whatever injured your elbow is necessary. Too much pickleball, tennis, computer typing got us into this elbow pain mess, so taking a break from it in the short term is necessary. The length of break that is required is dependent on the severity of the injury but can range from 2 to 12 weeks.
Step 2: Reset Your Elbow Muscles
Once your elbow pain has reduced, it is time to begin healing the muscles.
To get a head start on rebuilding your elbow strength, there are a number of exercises that we use at MOMENTUM Physical Therapy to help promote healing through the tendons on the outside of the elbow.
Here are two exercises to get you started:
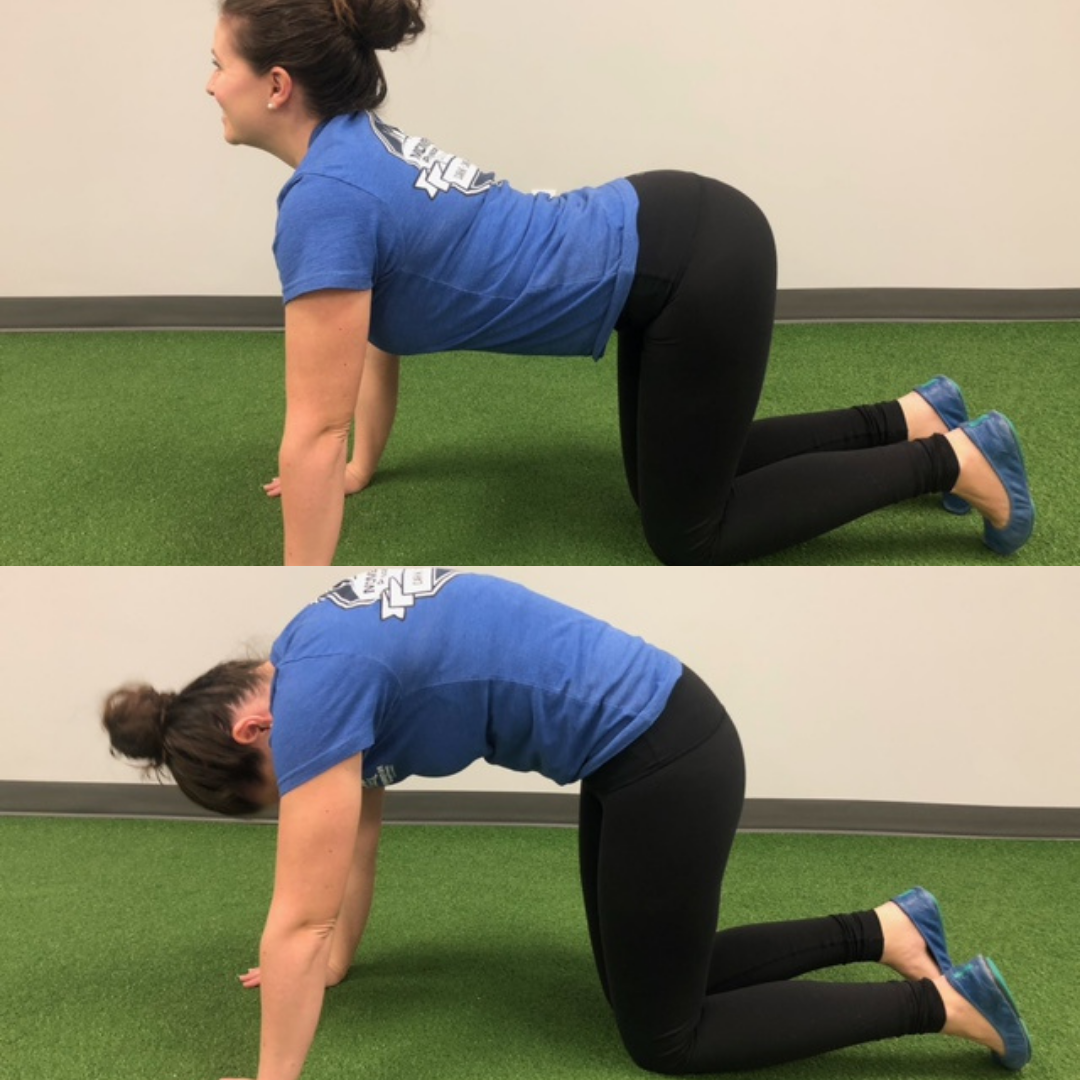
Eccentric Wrist Extension
Eccentric exercises involve lengthening a muscle while it's contracting. These types of exercises have been shown to be clinically beneficial for tendon-related injuries, like tennis elbow. Wrist extension exercises target the extensor muscles of the forearm, helping to strengthen and heal the injured tendons.
How To:
Sit on a chair with your forearm supported on a table, palm facing downwards.
Hold a light weight (such as a dumbbell or a can of soup) in your hand, with your wrist slightly bent.
Slowly extend your wrist by lifting the weight upward.
Then, lower the weight back down towards the ground in a controlled manner, taking around 6-8 seconds for this phase.
Repeat for 10-15 repetitions for 2-3 sets, gradually increasing the weight as tolerated.
Fatigue is ok, pain is not. Modify your reps and sets accordingly.
2. Forearm Extensor Stretch
Stretching exercises are used for improving flexibility, reducing muscle tension, and promoting blood flow. The forearm extensor stretch specifically targets the muscles and tendons on the outer part of the forearm, offering relief from tennis elbow pain.
How To:
Extend your affected arm straight out in front of you, with your palm facing down.
Use your other hand to gently bend your wrist downwards, towards the floor, until you feel a stretch along the outer part of your forearm.
Hold the stretch for 15-30 seconds, ensuring it's gentle and pain-free.
Relax and repeat the stretch 3 times, aiming for a total of 3 sets.
Step 3: See a Physiotherapist
Ready to kickstart your healing from tennis elbow? Seeing a Physical Therapist at MOMENTUM Physical Therapy in Okotoks will help speed up enhance your recovery journey. Tennis elbow recovery can be slow, so getting some professional help can speed up the process as a whole.
At MOMENTUM Physical Therapy, we recognize that each individual's journey to recovery is unique. Our skilled therapists employ a multifaceted approach to address tennis elbow, tailored to meet your specific needs and goals.
Here's how physical therapy can aid in your healing process:
Pain Management:
Managing pain is often the first step towards recovery. Our therapists utilize various techniques such as manual therapy, cupping, electrical stimulatiuon, or kinesiotaping to help enhance the pain reduction phase. There are additional exercises, depending on your presentation, that can help alleviate pain and reduce inflammation around the affected area.
2. Healing Promotion:
Kickstarting the healing process can help stimulate the body to speed up the healing process. Our physios use techniques that include soft tissue release, IMS (intramuscular simulation) for tennis elbow, and joint mobilizations to up regulate the bodies healing.
3. Stretching exercises:
Restricted range of motion can make tennis elbow worse and actually slow healing. Through hands-on physical therapy, IMS (intramuscular stimulation) for tennis elbow, stretching, and range of motion exercises, we work to restore flexibility and mobility in the affected area. This facilitates optimal healing while preventing future recurrences.
4. Strengthening Exercises:
Weakness in the forearm muscles can contribute to the development of tennis elbow. Through targeted strengthening exercises, we aim to improve the strength and endurance of these muscles. This will first promote healing and then will transition to injury prevention as your pain resolves.
5. Injury Prevention Education:
In many cases, improper technique or repetitive stressors contribute to the development of tennis elbow. Our therapists provide education on proper body mechanics and ergonomics tailored to your daily activities, helping you prevent further strain on the affected tendons.
Ready. Set. GO!
Taken as a whole, seeing a Physical Therapist at MOMENTUM Physical Therapy in Okotoks can dramatically improve the speed and effectiveness of your tennis elbow recovery.
Don't let tennis elbow keep you sidelined from the activities you love. With personalized care and expertise from MOMENTUM Physical Therapy, you can overcome this condition and regain full function of your elbow. Contact us today by calling 1-403-982-5600, or book online here, to schedule a first assessment and take the first step towards a pain-free future.
Our award-winning team here at MOMENTUM Physical Therapy- in Okotoks, is ready to help! Give us a call today at 403-982-5600 to get booked in with one of our awesome physiotherapists, massage therapists, or trainers. Or feel free to book online HERE!
We’re here for you!
Frequently Asked Questions
What is the best thing to do for tennis elbow?
Healing from tennis elbow requires a multistage process that includes pain reduction (ice), activity modification (rest), tissue healing, and progressive strengthening. Seeing a physical therapist is the best way to navigate these phases.
Can physical therapy help with tennis elbow?
Physical therapy is an effective treatment form for helping you recover from tennis elbow. Physical therapists are trained to treat tennis elbow and teach you how to heal the injured tendons.
How long does it take to recovery from tennis elbow?
Depending on how injured your elbow tendons are, recovery can range from 2-12 weeks.
Meet our Registered physiotherapists:
Meet our Kinesiologists:
Momentum Physical Therapy, located in Okotoks, Alberta, is ‘Here for YOU’.
If you are experiencing neck pain, have recurring headaches, or you just want to learn more about how massage therapy and physiotherapy can help heal your pain, don’t delay and call MOMENTUM Physical Therapy today. You can reach registered physiotherapists and massage therapists at MOMENTUM, located in Okotoks, by calling 403-982-5600. We look forward to helping you feel you best again.